Genomics: Insight
COVID 19: Common Misconceptions Addressed
Introduction
By now, everyone is familiar with the infamous virus: COVID-19. As the pandemic dominates media headlines and research publications, it’s difficult for everyday people to find reliable sources with accurate information. Naturally, unreliable or underdeveloped COVID-19 informational sources cause a wide variety of misconceptions about the pandemic today, including 1) our worries of a second wave, 2) the complexity behind a vaccine and 3) the possibility of going “back to normal” anytime soon in the United States. Some of the following information will be addressing the mentioned misconceptions and replacing them with reliable information that researchers and physicians have discovered thus far.
The Second Wave
With reinforcements of social distancing being made in various states around the country like Florida and Texas, the general public is concerned about whether the US might be enduring a harsher second wave of the pandemic. This is a valid concern as there was a brief time where rules were relaxed, but let’s dive deeper into why statistically, the Second Wave theory is a myth.
According to various articles published on PubMed, the current outbreak of COVID-19 is still classified as the “First Wave” because, in order for a “Second Wave” to occur, the first one has to die down completely. So why are people confused about this? Whilst looking at the daily COVID cases in the US, there are two peaks, at around mid-April and mid-July (Figure 1). However, a significant detail is that the dip in between these two months does not go down completely. It is understandable that a double peak graph of daily COVID cases can be misconceived as two waves, but it can only be considered that if the dip goes down to zero. As mentioned earlier, the “Second Wave” can only begin after the “First Wave has died down completely which, graphically, would be a dip that reaches zero.
The dip, however, is not the only detail that debunks the “Second Wave” myth. Taking a closer look at daily new cases per state, the trend does not show a double peak explaining a lot about whether there really is a second wave occurring. In Figure 2, there are two states, California and New Jersey, that were tracked on a similar timeline from March to August. Both states show a single peak in the number of COVID-19 cases across time, however, the drastic difference is that New Jersey had a major peak towards the beginning stages of COVID-19 in March and April, while California did not begin to reach its peak until late July. These differences in trends across states explain the apparent two peaks when the data is taken for the whole country. The graph of the US (Figure 1) takes the average number of new cases in all 50 states and ends up looking like a somewhat double-peaked graph. The double peak and dip to zero are the standard to determine that a certain region is facing a “Second Wave”, but a majority of the states that have been on the news have really only had one wave as of present. Due to the pattern of New York and New Jersey having major outbreaks in March/April and now Florida, Texas, and California climbing numbers rapidly while the other two states seem to be declining in cases, it is statistically inaccurate as of now to say the US is facing a “Second Wave”. However, no one is certain of what the future holds, so there is a possibility we could see one in the future.
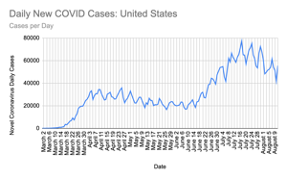
1) Number of COVID-19 cases across the United States from March to August 2020. The graph shows two peaks around mid-April and mid-July however, as the number of cases never dip to zero, the second peak is not considered a “Second Wave”. Graphed using data from World Charts on Google Sheets

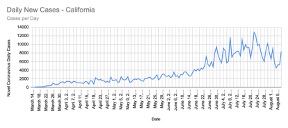
2) Number of COVID-19 cases in New Jersey (upper panel) and California (bottom panel) from March to August 2020. The number of COVID-19 cases in New Jersey peaked during mid-April showing only a “First Wave” while California experienced this trend later in July. These trends by state show that the United States had not experienced a “Second Wave”.
Challenges for the COVID-19 vaccine development
The vaccine for COVID-19 is a major topic of discussion as it is what determines the future of our country regarding the pandemic. However, to understand why it isn’t as simple as “just waiting for a vaccine,” one must understand the genomics of severe acute respiratory syndrome coronavirus 2 (SARS CoV-2), the strain of virus to which COVID-19 belongs. Learning about the evolution and molecular interactions of the frequently mutating single-stranded RNA virus will give insight into the complexity that people tend to overlook when talking about the vaccine and returning to “normal.”Challenges for the COVID-19 vaccine development
COVID-19 is a retrovirus, a virus that inserts their RNA genome into a host cell (i.e. human cell) and has the ability to use the host genome to encode for their viral proteins. SARS CoV-2 has a gene that encodes for a protein with a receptor-binding domain that allows for human to human transmission. Considering the error prone RNA polymerases (enzymes that build a DNA molecule) in human cells and the tendency for mutations to occur in the viral genome, the evolution of SARS CoV-2 may cause problems in vaccine development. To put it into perspective, the notorious HIV/AIDS is also a retrovirus like the coronavirus. The significance of this connection is that HIV has posed issues to researchers for decades with the constant evolution of its genome, making it hard for a single drug to stop the virus for long before it develops a resistant strain. There are already numerous strains and clusters of the coronavirus already, and to detect the new strains, scientists have to use other technologies like genome sequencing rather than the currently used ones such as polymerase chain reaction (used for COVID-19 detection). These factors can greatly increase the difficulty of containing or completely ridding the world of COVID-19.
The distribution of a safe vaccine in the US and going back to “normal”
A lot of the vaccine discussion has been geared towards the overarching topic of when things will get back to “normal.” Now that the genomic aspect and complexity has been explained, it is time to delve deeper into the complexity of actually distributing the vaccine to US citizens. On August 11th, 2020, Russia officially registered the first coronavirus ‘cure.’ Many US citizens are confused about how to feel about this announcement, so here are some facts that can contribute to whether this is a pro or a con.
For a vaccine to be available, it generally takes years considering in the past, the fastest developed vaccine was for mumps which took four years. The process for developing a traditional vaccine and during a pandemic can be seen in Figure 3. The key difference in the two processes is that the pandemic response for developing a vaccine involves overlapping stages, meaning manufacturing/distribution of the vaccine occurs despite the uncertainty that the vaccine is safe and effective. Additionally, the process is extremely expensive, costing hundreds of millions of dollars. These are major issues as accessibility to economically disadvantaged people will be decreased. Furthermore, an ineffective vaccine will cause major social issues further contributing to anti-vaccine propaganda. Also, if there are side effects to the unsafe vaccine, additional research will be needed to alleviate these medical issues.
That being said, many scientists have criticized the Russian vaccine because it has not been proven safe and effective. For such a vaccine, time is essential. Furthermore, Russia has not released much information about their vaccine, leaving many questions for the other countries. This also is indicative of how US citizens would get access to a vaccine developed in other countries. Even if the vaccine in Russia was proven effective and was approved for US citizens, distribution would be a whole other process in itself. Figuring out a way for lower class individuals to be vaccinated and determining the price of the vaccine would also play a major role. It is a huge misconception that an effective vaccine that can target the various strains of SARS CoV-2 and constantly be improved upon to contain the evolving, resistant strains, will be out by next year. Surely a vaccine could be proven effective somewhere on the planet, but US citizens being vaccinated and COVID-19 being completely contained within the next year is not a very probable scenario. Since there is so much that is out of our control, let us keep doing what is in our control by wearing functional masks and following social distancing guidelines.
Figure 3: Traditional vaccine development vs. COVID-19 vaccine development. Differently from the traditional vaccine development, in the pandemic vaccine development the process of manufacturing happens simultaneously with the processes of clinical development and safety/efficacy.
About the Author
Nitya Devisetti is a senior at Cupertino High School in Cupertino, CA. She has an immense interest in public health and community engagement, thus her decision to author an informative article aimed towards the general public.